Frequently Asked Questions - All FAQs

Yes, master social services and psychologists are covered by BeniComp Select, even if the services are not covered by the underlying plan.
Classes of eligible employees are different "levels" you have designated for the company. For example, you might create levels for:
Class 4: President
Class 3: C-level employees
Class 2: Executives
Class 1: Directors
Based on the levels you designate, you assign a certain number of employees to each class.
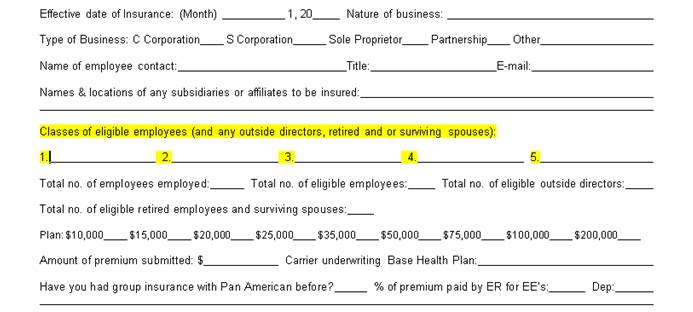
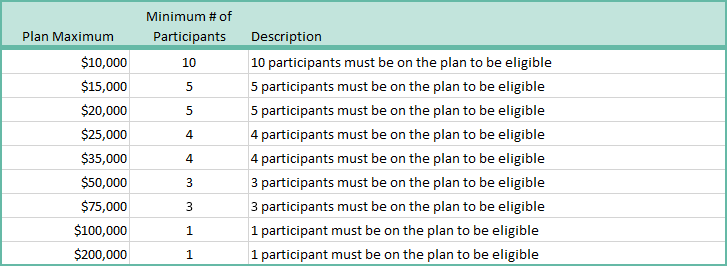
Please refer to the chart below. Based on the number of participants you have on the total plan, you can assign the number of participants to classes with corresponding plan maximums. For example, if you have 15 employees on BeniComp Select, you might have:
Class 4: 1 President with a plan maximum of $25,000
Class 3: 2 C-level employees with a plan maximum of $20,000
Class 2: 4 Executives with a plan maximum of $15,000
Class 1: 8 Directors with a plan maximum of $10,000
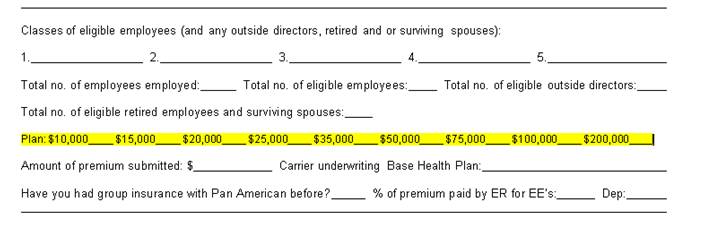
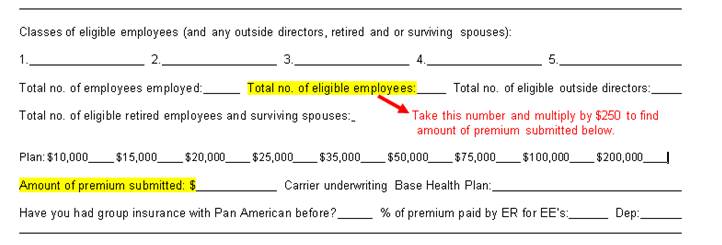
The application premium is the total number of participants multiplied by $250. For example, if you have 10 participants on BeniComp Select, then the premium check submitted with the application should be $2,500.
Yes, we support Apple products. By default, the Safari browser blocks pop-up windows. See below:
When you are on your iPhone, the safari browser defaults to no pop-ups.
- Go to Settings and scroll down to Safari
- Click on Safari and un-check Block Pop-Ups
- When you try the dropdown again it will prompt you: This site is attempting to open a pop-up window
- Click Allow
No, this policy can be placed on as few or as many employees, based on class, as the company chooses. Further, the company has the option of choosing different benefit levels on different classes of employees. Classes are determined by the company. If a policy is being offered to a class, everyone eligible for the designated class must be offered the plan.
A BeniComp Select policy does not have an age limit or a waiting period.
Generally, if an expense is medically necessary and qualifies under Section 213 (d) of the Internal Revenue Code, it is eligible for reimbursement. Elective procedures that are not medically necessary are not covered by BeniComp Select.
Supporting documentation must be included with any expense submitted for reimbursement. The Explanation of Benefits (EOB) supplied by the primary plan needs to be included with every medical claim to show the services provided went through the primary plan first. If the service provided is explicitly not covered by the primary plan, please submit the Summary Plan Description explaining the service is not covered.
Further examples of supporting documentation include, but are not limited to:
- Explanation of Benefits (EOB) from the primary plan, including reason(s) for denial
- Itemized Receipts and/or Bills are required for services not covered by the primary plan
- Letter of Medical Necessity if applicable
- Superbills or Physician Receipts are acceptable for co-payment amounts provided they include patient name, date of service, and co-payment amount
- Prescription Drug Receipts must include patient name, name of prescription, date the prescription was filled and co-payment amount, if applicable
All supporting documentation, including photocopies, must be legible and include the patient's name, date and type of service, and the dollar amount.
Claims cannot be processed from:
- Balance forward/due statements
- Charge card receipts
- Cancelled checks
No, you do not need to upload each claim item's supporting documentation separately. You can upload all of the supporting documentation one time under Supporting Documentation Upload.


